With XBB variant emerging in Singapore, another COVID-19 wave has come upon our shores.
On Tuesday (18 Oct), there were 11,934 new infected cases, reported the Ministry of Health (MOH).
Currently, 662 COVID-19 patients are hospitalised. Of these, 58 require oxygen supplementation and 14 patients that are in Intensive Care Units (ICU).
Although the spiking daily caseload is worrisome, it is not the main reason for the longer waiting times for hospital admission, or for the high occupancy rate of hospital beds.
Longer Waiting Times
According to CNA, the waiting time for admission at hospitals can be as high as 50 hours, as public emergency departments continue to see a high number of patients.
Ng Teng Fong General Hospital and Sengkang General Hospital, in particular, have waiting times of up to 50 hours.
We joke about Singaporeans randomly joining long queues a lot because we are kiasu, but this… This is not the type of queue anyone wants to see.
The latest data from MOH’s website shows that the median waiting time for admission to wards from emergency departments was between one hour and 24.2 hours for the last week of September.
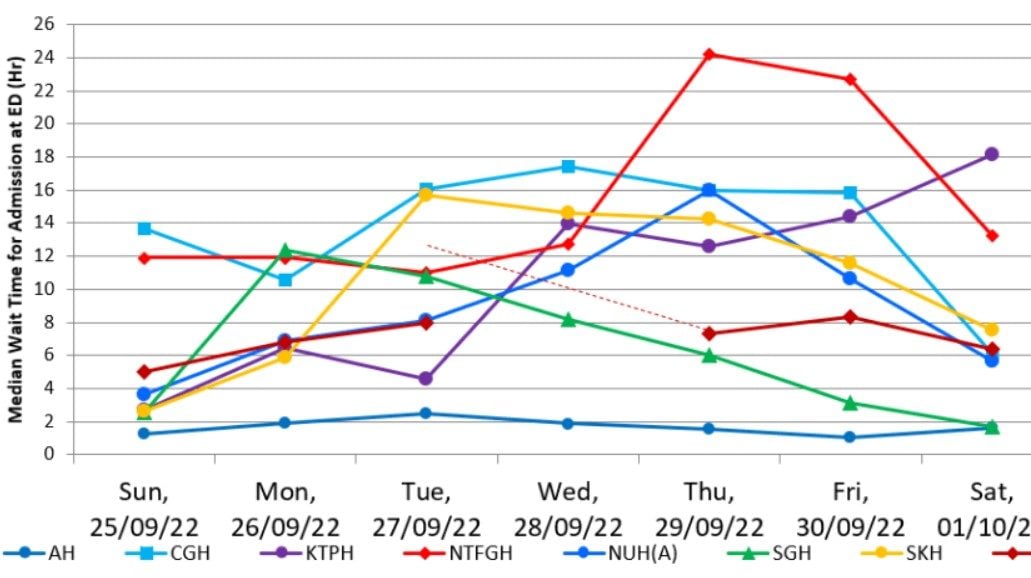
It is lower but having to wait more than a full day is terrible too.
The Lapse of Severe Illnesses
So what is causing these longer waiting times?
There’s actually a few factors, but the main cause is the increase in patients with severe illnesses.
For inexplicable reasons, a lot of seniors have chosen to let their own medical conditions fall to the wayside during the COVID-19 pandemic.
Instead of going to general practitioner doctors to get their ailments checked out or have their medications refilled, these older people simply did nothing.
Therefore, the people who are being admitted into the hospital now are sicker and they need to be hospitalised.
This is incredibly stressful for the family members of these older patients too.
They are made to wait long hours before their older parents are given a hospital bed, but they cannot accompany the patients because of the stricter safe management measures.
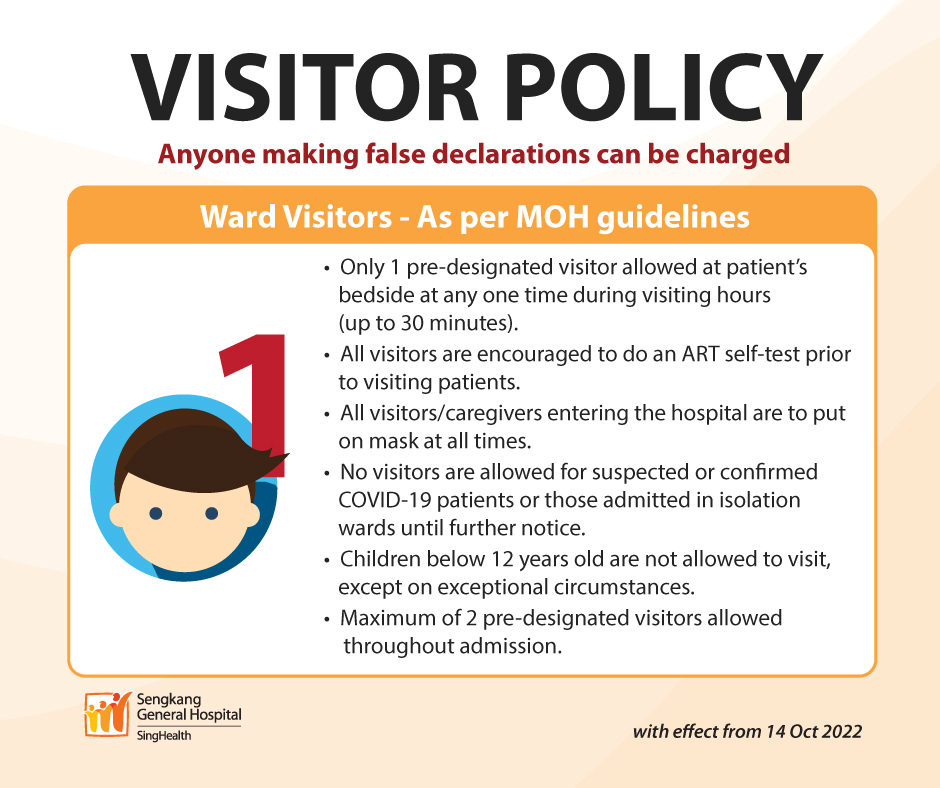
As a matter of fact, some public hospitals are so crowded that beds are even spilling into the hall, said Ms Lim, whose mother was warded in the Ambulatory Surgery Centre.
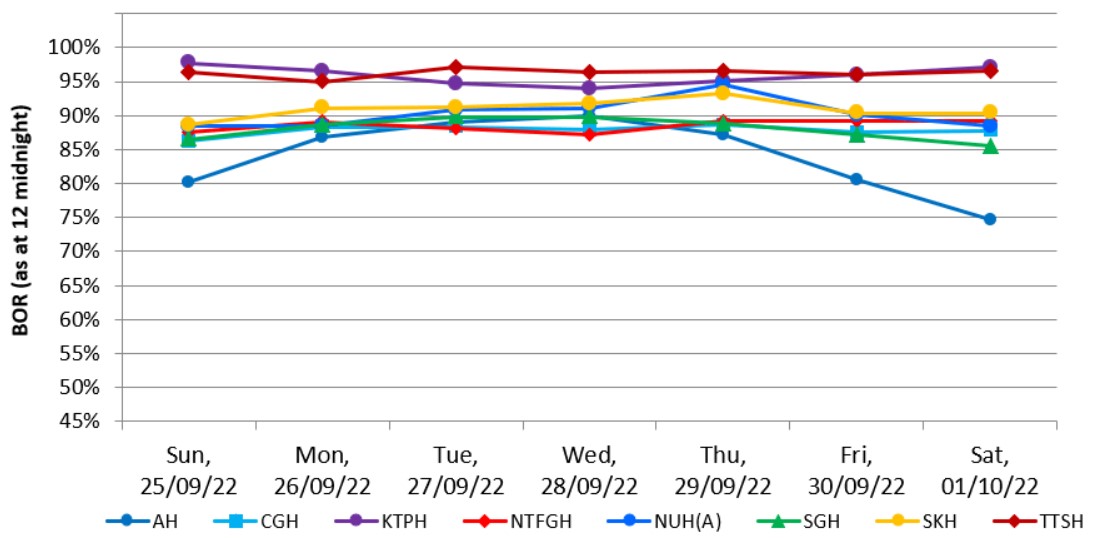
This is supported by the bed occupancy rates provided by the Health Ministry, which show that bed occupancy rates range between 74.7% to 97.6% between 25 September and 1 October.
Manpower, Flu, and COVID-19
The next three factors are correlated.
Due to the more staff members testing positive in the new wave of COVID-19 cases, more healthcare workers are going down for the count.
Reportedly, a lot of junior doctors have had to call in sick, to the extent where the hospitals are grasping at straws because they have no one to recall to help with the surging number of patients.
The senior doctors and those uninfected are then forced to cover for them, but long shifts in crowded hospitals are exhausting. One doctor describes it as an “endless vicious cycle”.
Worse, these doctors will also collapse and fall ill out of exhaustion.
Besides the ongoing COVID-19 pandemic, the usual flu season has come upon us.
Ergo, there are more patients coming to the emergency department with symptoms that are similar to the coronavirus.
And therein lies another problem: while antigen rapid tests (ART) and polymerase chain reaction tests (PCR) are able to identify a positive infected case, it can take time for the infection to reach the upper portions of our nose and throat where we swab to test.
Some Omicron variants are also capable of avoiding detection because they don’t cause the S gene target failure which triggers a positive reaction from the PCR.
But hey, it’s better safe than sorry right?
Whether it is normal flu or COVID-19, getting diagnosed by a hospital doctor is definitely more accurate.
This, in turn, increases the number of people waiting for admission at hospitals.
As such, the ministry is urging members of the public to go to the hospital emergency only if it is an emergency.
“We also appeal to everyone to play their part in alleviating the load on our public hospitals by visiting the general practitioner or polyclinic doctor first if they are experiencing mild respiratory symptoms and/or non-life-threatening conditions,” said the spokesman from MOH.
If this message sounds familiar, it’s because the Health Ministry has said the same words during each wave of COVID-19.
Featured Image: Google Maps